Bladder Health After 50
What's Normal, What's Not, and When to Talk to Your Doctor

Let’s talk about something many women over the age of 50 experience, but rarely discuss: unexpected bathroom urgency, occasional leaks, incontinence, or recurring UTIs. These changes can feel isolating or embarrassing, but they’re incredibly common—and there are real, evidence-based solutions.
Below, we break down what’s happening in your body after menopause, how symptoms can differ, and where to start the conversation with your healthcare provider.
Why menopause can change urinary health
During and after menopause, estrogen levels fall. That drop can weaken urogenital muscles, make it harder to fully empty the bladder, and contribute to prolapse—each of which can drive frequency and leaks. Estrogen also supports a protective vaginal and urinary ecosystem. When it declines, beneficial lactobacilli decrease and pH can rise, creating conditions where potentially harmful microbes may grow—raising Urinary Tract Infection (UTI) risk.
What can help (to discuss with your clinician):
- Adjust day-to-day habits that may irritate the bladder (for example, consider limiting common irritants like caffeine and alcohol) and build in time to fully relax on the toilet so the bladder empties more completely.
- Ask whether pelvic support options are appropriate if prolapse is contributing to symptoms.
- Post menopause, ask your clinician whether topical vaginal estrogen could support local defenses and help reduce recurrent UTI risk; benefits may lessen if therapy stops, so plan for follow-up.
OAB, incontinence, or UTI? How to tell the difference
Symptoms overlap, but these conditions aren’t the same. Understanding the basics helps you describe what you’re feeling to your provider:
- Overactive bladder (OAB): sudden, hard-to-ignore urge to urinate; frequent trips—even when the bladder isn’t full. “Normal” urinary frequency is about seven times during waking hours.
- Urinary incontinence (UI): involuntary urine leakage; may occur with cough/laugh/lift (stress), with sudden urges (urge), from incomplete emptying (overflow), or due to mobility/cognitive barriers (functional).
- UTI: a bacterial infection often causing burning with urination, frequent urges, and other classic signs; requires medical diagnosis and treatment.
Because symptoms can look similar, especially after 50, get a proper evaluation rather than self-diagnosing.
What can help (to discuss with your clinician):
- For OAB and many forms of UI, first-line approaches include bladder training and behavioral strategies (e.g., structured bathroom schedules, urge-suppression techniques, and practical changes to reduce irritants).
- If leakage happens with exertion (cough/laugh/lift), ask about pelvic floor strengthening approaches and whether additional supports are appropriate for your situation.
- If burning, pain, or cloudy/strong-smelling urine appear, ask about testing and treatment for UTI rather than self-treating.
What’s typical after 50?
- More frequent bathroom trips (and sometimes leaks). Aging and lower estrogen reduce bladder stretch and muscle efficiency, so the bladder may fill more often and empty less completely driving frequency and leaks. Prolapse can contribute.
- A higher risk of recurrent UTIs. Postmenopausal changes in the vaginal microbiome increase susceptibility to UTIs; recurrent UTIs can become more challenging with age.
- In older adults, symptoms can look different. Some elderly adults may not feel the classic UTI burning/urgency; instead, UTIs may present as confusion or changes in thinking—another reason to involve a clinician early when something feels “off.”
What can help after 50 (to discuss with your clinician):
- For frequency/leaks, try behavioral adjustments (allow more time to void, plan bathroom breaks, and reduce common irritants) and ask whether pelvic support is relevant if prolapse is suspected.
- For recurrent UTIs after menopause, ask about topical vaginal estrogen as a targeted option and create a plan for monitoring benefits and side effects over time.
- For older adults, caregivers should watch for sudden changes in thinking/behavior and ask about appropriate testing when UTI is suspected.
Evidence-based options to discuss with your healthcare provider
Your clinician can help you pinpoint what’s going on and tailor a plan. Approaches discussed in the provided resources include:
Here are a few behavioral strategies for OAB/UI:
- Bladder training (timed voiding and urge-delay techniques).
- Take time to fully empty—don’t rush.
- Reduce bladder irritants like caffeine and alcohol as needed.
These can be effective first steps before moving to procedures or prescriptions.
- Medical therapies for OAB (when needed): Your provider may consider medications and, when appropriate, procedural options such as nerve stimulation or targeted injections; surgery can be a later-line option for select cases.
- UTI diagnosis and treatment: UTIs generally require clinical evaluation and antibiotics when indicated; early care helps prevent complications. Avoid self-treating without guidance.
- Vaginal estrogen for UTI (post menopause): Topical vaginal estrogen can help restore local pH/microbiota and may reduce recurrent UTI risk; benefits may decline if therapy stops, so ongoing follow-up is helpful.
When to call your healthcare provider
- New or worsening urinary urgency, frequency, or leaks that affect daily life.
- Classic UTI symptoms (burning with urination, frequent urges, cloudy/strong-smelling urine, lower abdominal discomfort, blood in urine).
- Confusion or sudden changes in thinking/behavior in older adults, which can be a UTI red flag.

Taking control of your urinary health after 50
Understanding what’s happening in your body is the first step. The second is having an honest conversation with your healthcare provider about what you’re experiencing—no matter how uncomfortable the topic might feel.
And remember you don’t have to wait for symptoms to worsen. Proactive steps like staying hydrated, managing bladder irritants, and considering science-backed UTI prevention products like Uqora can help you take control of your urinary health before issues escalate.
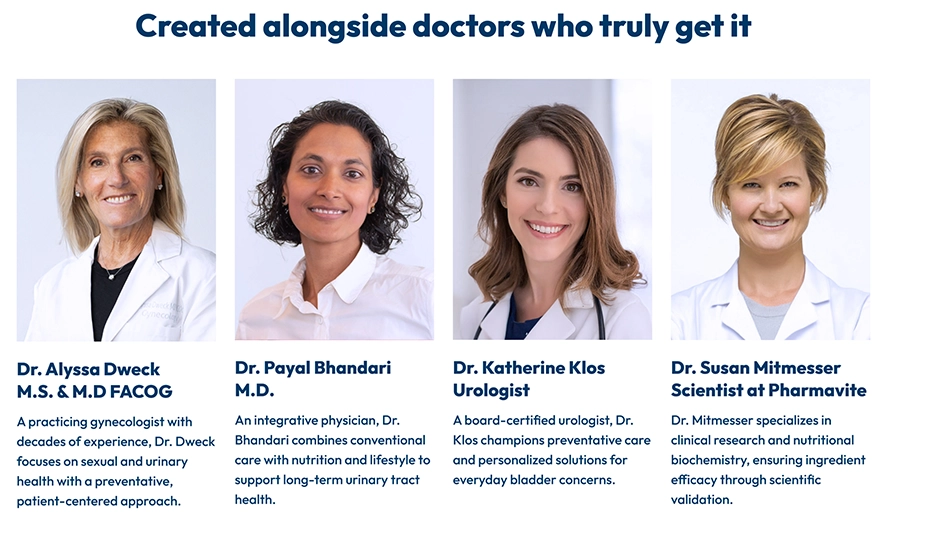
Uqora was created alongside doctors who truly get it—board-certified urologists, gynecologists, and scientists specializing in urinary tract health who understand the real challenges women face and the solutions that actually work.
Learn more about Uqora’s UTI prevention products and how they support urinary health after 50 at Uqora.com.